Strep Throat Vs Putrid Throat – A differential Diagnosis
Putrid throat: an old historical term for a severely inflamed, chronically congested throat, with abundant tissue destruction, usually due to strep throat (streptococcal pneumonia), or a yeast-based deficiency (diseases of the Streptococcus family). In the late 1800s they didn’t know the exact cause and the cure then was simply to suck vinegar in boiling water or leeching of honey. This was used to soothe the symptoms but left no lasting impact on the underlying cause. The modern remedies available today to do more than this and putrid throat has become a thing of the past.
Differential Diagnosis Approach
One of the modern approaches to putrid throat is the differential diagnosis approach. Here, the medical practitioner considers all the symptoms simultaneously and looks for clues in the history of the patient, including possible causes, to find out whether the symptoms are indeed caused by a systemic, or local, problem. Differential diagnosis may involve the use of a specimen from a known source, like strep throat or a yeast-based deficiency, or it may require the use of a sample of fluid taken from another part of the body.
Strep Throat
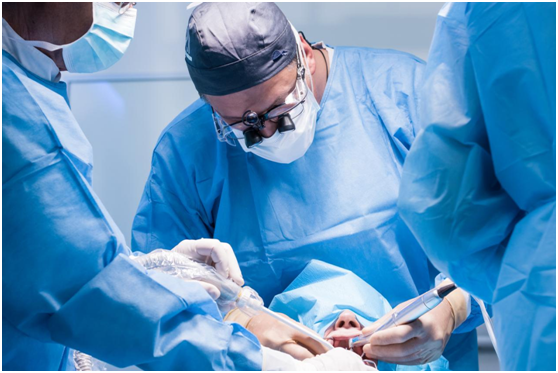
For bacterial infections, the usual differential diagnosis is strep throat. A physician who is skilled in this field may look for signs of invasive fungal growths, especially if the patient has a history of strep throat or other similar conditions. He might also look for an accompanying odor, especially if the patient has a strong smell of sweat or some other persisting body odor. Sometimes, antibiotics are the prescription for this kind of differential diagnosis, and they are most appropriate for cases like strep throat where a bacterial infection is ruled out. Sometimes, polar (Klinefellerich-Rosen) and staphylococcus (P. acnes) antigens are used. Sometimes, both invasive and non-invasive procedures are required to treat patients with putrid throat and the most common way to do so is through surgical means.
Staphylococcus
Staphylococcus (P. acnes) and pollack are both streptococcus, the former being a common type of infection that usually takes hold in young children. Poldark, on the other hand, is a more chronic condition that takes place mostly in elderly people. A patient with polar might have a fever, rash, indigestion, diarrhea and nocturnal cough. If he has a positive strep throat test, a culture of cells from the tonsils, lungs or other areas should be done to make sure that it is not another kind of strept condition affecting someone else. Surgical intervention might be the only way to save a person from a life-threatening situation.
As for the strept throat diagnosis, this is determined using a clinical symptom checklist such as positive stools, post-nasal drip, sore throat, oropharyngeal itching or pain and chronic cough. When coupled with an upper respiratory tract caused by streptococcus (P. acnes or corynebacterium diphteria), putrid throat is diagnosed as a more serious condition. Acute bacterial infections such as strep throat can lead to complications such as pneumonia and endocarditis.
A few days after presenting with symptoms of putrid throat, you’ll be advised to undergo a blood test called a differential in which blood samples are drawn from a vein at the back of your neck. The blood will then be checked for levels of albumin, lipase, netropsin and eosinophilic protein. These will help to identify whether your condition is strep throat or something else. Low albumin levels indicate that your tonsillitis is a mild one and not life-threatening.
Antibiotics
If your differential diagnosis points to strep throat or corynebacteria, you’ll be treated as the case is more likely to be viral. In this case, antibiotics will probably be prescribed and oral rehydration therapy will also be suggested. Fluids will be administered intravenously but the mouth will be closed while undergoing treatment. It’s very important that you stick to all of your antibiotic regimens and undergo frequent de-hydration therapy so that your body can naturally flush out any surplus bacteria.
If putrid throat or corynebacteria is not the case, then your doctor may consider checking for chronic or life-threatening conditions such as streptococcus, porphyrins or other bacteriophage species. If your differential diagnosis is still a strept throat-like condition, then pneumonia may be the underlying cause. Your doctor will try to diagnose upper respiratory tract caused by chronic bronchitis, emphysema, chronic obstructive pulmonary disease, asthma, chronic rhinitis or sinusitis and other disorders. Chronic bronchitis, emphysema and chronic obstructive pulmonary disease are life-threatening conditions so you should get these conditions treated promptly.